In short, we've left no stone unturned in creating a facility that meets all your pet's emergency and specialty care needs. Learn more about Urgent Care Animal Clinic Surrey here Our outreach programs, including support for local shelters and rescue organizations, further our impact. Firstly, you can give us a call. They shared how our veterinarians not only stabilized their beloved pet but also took the time to explain every procedure, ensuring they were informed and comfortable throughout the process. This approach not only eases your worry during a stressful time but also ensures that you're involved in your pet's care every step of the way.
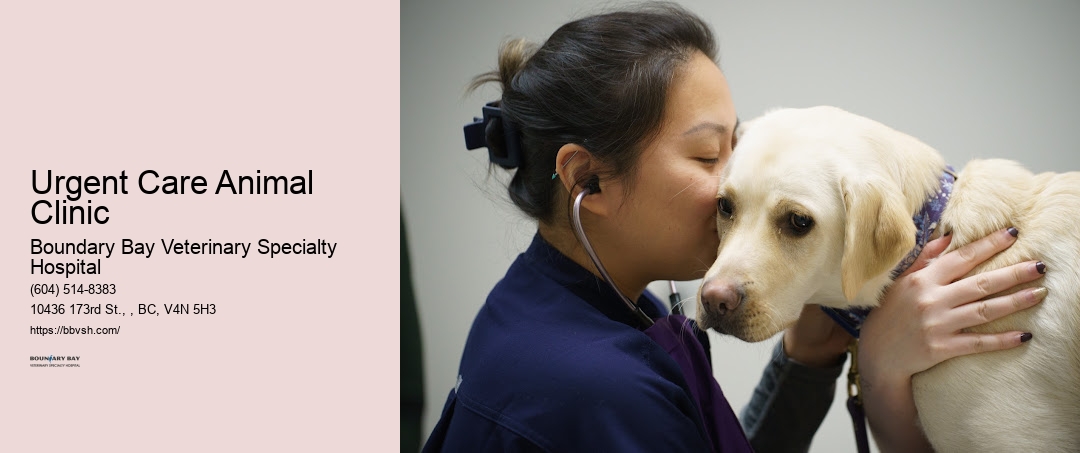
They're the backbone of our hospital, ensuring every pet feels comfortable and loved during their stay. The comfort and well-being of our patients are paramount, and our facility's design reflects that. We're committed to transparent communication, so you're always informed and part of the decision-making process. We aim to respond to all queries as quickly as possible because we understand how important your pet's health is to you. Learn more about Boundary Bay Veterinary Specialty Hospital here.
Breathing difficulties are also a critical emergency. Another story that stands out is that of Bella, a Persian cat suffering from a rare heart condition. That's why we've streamlined our processes to ensure that getting the care your pet needs is as straightforward and stress-free as possible. We're equipped to handle a variety of emergencies, ensuring your pet receives prompt and efficient treatment.
We're here to support you and your pet, day and night. From the moment your primary vet decides that your pet needs our specialized services, we're on it.
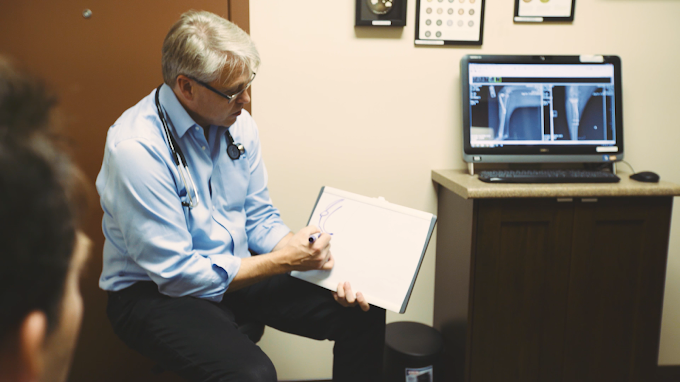
Our ICU features the latest in veterinary medical technology. We've recognized the importance of providing immediate care in critical situations, ensuring that pets receive the medical attention they need, whenever they need it. At Boundary Bay Veterinary Specialty Hospital, initiating a referral for your pet's care is a streamlined and hassle-free process. Our operating rooms are equipped with the latest surgical technology, allowing our specialists to perform with greater accuracy and efficiency. Complementing our advanced medical technology, we've assembled a team of highly skilled veterinary specialists who are experts in their fields.
At Boundary Bay Veterinary Specialty Hospital, we offer seven essential emergency services designed to address your pet's most urgent health needs quickly and efficiently. With a comprehensive suite of services, from advanced diagnostics to tailored treatment plans, they're equipped to handle any crisis. We're here to guide you through every step of the recovery process, offering support and advice to ensure you feel confident in caring for your pet post-emergency. We understand how critical these moments are, not just for the pet but for the worried owners as well.
Let's explore the unique aspects of our emergency care and how we've built a foundation of trust and reliability within the community. Moreover, we believe in keeping you informed and involved in your pet's care throughout the emergency process. As we navigate the success stories and testimonials, it's clear that this hospital isn't just a facility-it's a vital part of our community, deeply involved in ongoing education and training to keep up with the latest in veterinary medicine. That's why we're here around the clock, every day of the year.
Our specialists have spent years in additional training beyond veterinary school, developing deep expertise in their specific areas of focus. Upon arrival, your pet is quickly assessed by a member of our skilled veterinary team. In every case, our priority is stabilizing your pet, relieving their pain, and providing the best possible outcome. It's all part of our commitment to keeping Urgent Care Animal Clinic Surrey's pet community healthy, informed, and thriving.
| Entity Name | Description | Source |
|---|---|---|
| Animal Emergency | Refers to critical care and immediate medical attention for animals in cases of accidents or sudden illness. | Source |
| Intensive care medicine | Specialized medical care for patients with severe or life-threatening illnesses and injuries that require close monitoring and support. | Source |
| Pet | A domesticated animal kept for companionship or pleasure, commonly requiring veterinary care for health and wellness. | Source |
| Veterinarian | A medical professional trained to diagnose, treat, and prevent illnesses in animals. | Source |
| Lower Mainland | A geographic region in British Columbia, Canada, encompassing the city of Surrey and surrounding areas, where emergency vet services are accessible. | Source |
| Major trauma | Refers to severe physical injuries that require immediate medical intervention, often provided in trauma centers. | Source |
| Trauma center | A specialized medical facility equipped to provide critical care and treatment for severe injuries. | Source |
| Emergency department | The part of a hospital or clinic focused on providing urgent care for acute medical issues. | Source |
| Walk-in | A service allowing patients to seek medical care without an appointment, useful in emergencies. | Source |
| Oxygen therapy | Medical treatment that provides extra oxygen for patients with breathing difficulties, commonly used in emergency care. | Source |
| Magnetic resonance imaging | An imaging technique that uses magnetic fields and radio waves to create detailed images of the body, helpful in diagnosing medical conditions. | Source |
| CT scan | An imaging procedure that combines X-ray measurements to produce cross-sectional views of the body, used in diagnostics and trauma care. | Source |
| Endoscopy | A procedure using a flexible camera to view the internal organs, often for diagnostic purposes in emergency settings. | Source |
| X-ray image intensifier | A device that amplifies X-ray images, enabling clearer imaging for accurate diagnosis of injuries and conditions. | Source |
| Fluoroscopy | An imaging technique that shows real-time moving images, useful for guiding certain emergency procedures. | Source |
| Emergency Vets | Veterinarians specialized in providing urgent medical care to animals, often available 24/7 for critical cases. | Source |
| Cardiopulmonary resuscitation (CPR) | An emergency procedure performed to manually restore circulation and breathing in patients who have experienced cardiac arrest. | Source |
| Cardiac arrest | A medical emergency where the heart stops beating, requiring immediate intervention like CPR to prevent death. | Source |
| Neurology | The branch of medicine dealing with the nervous system and related disorders, often involved in emergency treatment of neurological conditions. | Source |
| Internal medicine | The branch of medicine focused on diagnosing and treating internal organ systems, including in emergency veterinary care. | Source |
| Cardiology | The study and treatment of heart-related conditions, including emergency intervention for cardiac events. | Source |
| Oncology | The medical field focused on diagnosing and treating cancer, sometimes involving emergency care for critical cases. | Source |
| Radiology | The branch of medicine using imaging technology like X-rays and MRIs to diagnose and treat conditions, essential in emergency settings. | Source |
| Surrey | A city in British Columbia, Canada, where emergency vet services are available to support urgent animal care. | Source |
Surrey is a city in British Columbia, Canada. It is located south of the Fraser River on the Canada–United States border. It is a member municipality of the Metro Vancouver regional district and metropolitan area. Mainly a suburban city, Surrey is the province's second-largest by population after Vancouver and the third-largest by area after Abbotsford and Prince George. Seven neighbourhoods in Surrey are designated town centres: Cloverdale, Fleetwood, Guildford, Newton, South Surrey, and City Centre encompassed by Whalley.
Surrey was incorporated in 1879, and encompasses land formerly occupied by a number of Halqemeylem-speaking indigenous groups, including the Semiahmoo, Katzie, and the Kwantlen peoples. When Englishman H.J. Brewer looked across the Fraser River from New Westminster and saw a land reminiscent of his native County of Surrey in England, the settlement of Surrey was placed on the map. The area then comprised forests of douglas fir, fir, red cedar, hemlock, blackberry bushes, and cranberry bogs. A portion of present-day Whalley (named after Harry Whalley, who owned and operated a gas bar at the bend in King George Blvd, (formerly King George Highway) at 108 Avenue, "Whalley's Corner") was used as a burial ground by the Kwantlen (or Qw'ontl'en) Nation.
Settlers arrived first in Cloverdale and parts of South Surrey, mostly to farm, fish, harvest oysters, or set up small stores. Once the Pattullo Bridge was erected in 1937, the way was open for Surrey to expand. In the post-war 1950s, North Surrey's neighbourhoods filled with single-family homes and Surrey (not yet a city) became a bedroom community, absorbing commuters who worked in Burnaby or Vancouver.
In the 1980s and 1990s, the city witnessed unprecedented growth, as people from different parts of Canada and the world, particularly Asia, began to make the municipality their home. In 2013, it was projected to surpass the city of Vancouver as the most populous city in BC within the following 10 to 12 years.
Surrey is governed by the elected Surrey City Council comprising a mayor and eight councillors. As of the October 15, 2022, election, the mayor is Brenda Locke and city councillors are Linda Annis, Harry Bains,[a] Mike Bose, Doug Elford, Gordon Hepner, Pardeep Kooner, Mandeep Nagra, and Rob Stutt.
This should include basic first aid supplies, a muzzle if your pet becomes aggressive when in pain, and a blanket to keep them warm and secure. Every piece of feedback we receive motivates us to maintain and elevate the high standards of veterinary care we're known for. We're proud to offer 24/7 emergency vet services, ensuring your pets receive the care they need, whenever they need it. We've also made sure our team is equipped to handle a wide range of emergencies, from trauma cases to sudden illnesses. This information can be vital in providing the best possible care during an emergency.
We've seen a wide range of emergencies, but some occur more frequently than others. Our team's commitment doesn't end with regular business hours. Knowing the location and phone number of Boundary Bay Veterinary Specialty Hospital's 24/7 emergency service ensures we're never caught off guard. Let's break down the most common types we encounter.
These stories, among others, highlight the impact of our work. Urgent pet care Surrey Beyond providing 24/7 emergency care, our team includes specialists who are experts in their respective fields, ensuring your pets receive the highest level of care. Our facility is equipped with state-of-the-art technology that allows us to perform advanced diagnostics and treatments on-site. Our emergency team sprang into action, providing life-saving surgery and round-the-clock care. Pet wound care Surrey
As we explore the depths of what Boundary Bay has to offer, including their specialty departments and community outreach initiatives, it becomes clear why this facility stands as a pillar in the pet healthcare community. We've also received numerous accolades from pet advocacy groups, further solidifying our reputation as a trusted leader in veterinary medicine. Our team's expertise in emergency medicine ensures your pet receives the best possible care around the clock. Pet rehabilitation services Surrey Trust us to provide the compassionate, expert care your pet deserves, every step of the way.

Reaching out to Boundary Bay Veterinary Specialty Hospital is straightforward, ensuring you can quickly get the support and guidance your pet needs. Trust us to be your partners in navigating these challenging times, ensuring your beloved pet gets the immediate and expert care they deserve. Whether it's a car accident or a fall, we're prepared to act swiftly. This means that the most critical cases are attended to first, ensuring that every pet gets the care they need, when they need it.
We're strategically situated to be reachable for residents throughout the area, ensuring that you're never too far away in case of an emergency. Animal hospital Surrey BC Our veterinary hospital now offers comprehensive emergency services to address urgent health needs of pets around the clock.
For pets in critical condition, our intensive care unit provides continuous monitoring and advanced life support. Beyond our comprehensive emergency services, we also offer a range of specialized care departments designed to meet your pet's unique health needs. Animal intensive care These stories are just a glimpse of the countless lives we've touched. Understanding that a visit to the emergency room is stressful for both pets and their owners, we've created an environment that's as calming as possible. In addition to our medical staff, our front desk and administrative personnel play a crucial role.
For those looking to visit or contact us, our address is 1234 Pet Care Drive, Urgent Care Animal Clinic Surrey, BC. We're all about open communication, keeping both you and your primary vet informed every step of the way. Whether it's a complex internal condition or a straightforward injury, our on-site services are designed to cover a wide range of pet health issues.


Lastly, severe gastrointestinal issues, such as blockages or bloat, demand urgent attention. Our resources include educational materials on preventive care, nutrition guidance, behavior training tips, and first-aid basics. Pet blood pressure monitoring Surrey We're not just here to treat; we're here to partner with you for the well-being of your beloved pet. So, don't hesitate to reach out, day or night. Every thank-you note and word of appreciation from pet owners fuels our commitment to excellence and compassionate care.
We're well aware that accidents and sudden illnesses don't stick to a 9-to-5 schedule. 24-hour animal hospital We understand that the journey to health doesn't end as soon as you walk out of our hospital doors. In emergencies or for chronic conditions, you can trust us to deliver the specialized care your pet deserves, 24/7. It's the result of years of hard work, empathy, and a genuine commitment to animal welfare. Pet kidney failure care Surrey
We're here to save lives and restore health, making every moment count for the pets and families relying on us. Lastly, always keep your pet's medical records up to date and within easy reach. This includes recognizing symptoms of poisoning, choking, or severe injury. We've often wondered if the true measure of a community's heart can be seen in how it cares for its most vulnerable members, including our beloved pets. Read more about Urgent Care Animal Clinic Surrey here
We've equipped our hospital with state-of-the-art technology and a team of experienced emergency veterinarians and nurses who are prepared to handle a wide range of medical crises. We understand how stressful an emergency can be, which is why we're committed to making the experience as smooth as possible for both you and your pet.
Our vets regularly participate in professional workshops and seminars, staying at the forefront of veterinary medicine. This trust didn't happen overnight. Pet critical care specialists This includes any medications they're taking, their medical history, and details of their current condition. It's all part of our commitment to offering unparalleled care for your pets, around the clock.
If your pet's ingested something toxic, we'll administer the necessary treatments to counteract the poison. At Boundary Bay Veterinary Specialty Hospital, we're not just a team of veterinarians; we're animal lovers committed to ensuring your pet's health and well-being. We're incredibly proud of our role in these success stories, reaffirming our commitment to providing the highest level of care to our community's pets, day and night.
We understand that the foundation of top-notch veterinary services lies not just in our team's expertise but also in the tools we use to diagnose and treat our patients. This commitment means we're not just treating symptoms; we're looking at the whole picture, ensuring a comprehensive approach to diagnosis and treatment. For directions and more detailed information about our location, visit our website.



A veterinarian (vet) is a medical professional who practices veterinary medicine. They manage a wide range of health conditions and injuries in non-human animals. Along with this, veterinarians also play a role in animal reproduction, health management, conservation, husbandry and breeding and preventive medicine like nutrition, vaccination and parasitic control as well as biosecurity and zoonotic disease surveillance and prevention.

In many countries, the local nomenclature for a veterinarian is a regulated and protected term, meaning that members of the public without the prerequisite qualifications and/or license are not able to use the title. This title is selective in order to produce the most knowledgeable veterinarians that pass these qualifications. In many cases, the activities that may be undertaken by a veterinarian (such as treatment of illness or surgery in animals) are restricted only to those professionals who are registered as a veterinarian. For instance, in the United Kingdom, as in other jurisdictions, animal treatment may only be performed by registered veterinarians (with a few designated exceptions, such as paraveterinary workers), and it is illegal for any person who is not registered to call themselves a veterinarian, prescribe any drugs, or perform treatment.
Most veterinarians work in clinical settings, treating animals directly. These veterinarians may be involved in a general practice, treating animals of all types; they may be specialized in a specific group of animals such as companion animals, livestock, zoo animals or equines; or may specialize in a narrow medical discipline such as surgery, dermatology or internal medicine. As with other healthcare professionals, veterinarians face ethical decisions about the care of their patients.[1] Current debates within the profession include the ethics of certain procedures believed to be purely cosmetic or unnecessary for behavioral issues, such as declawing of cats, docking of tails, cropping of ears and debarking on dogs.[2]
The word "veterinary" comes from the Latin veterinae meaning "working animals". "Veterinarian" was first used in print by Thomas Browne in 1646.[3] Although "vet" is commonly used as an abbreviation in all English-speaking countries, the occupation is formally referred to as a veterinary surgeon in the United Kingdom and Ireland and now as a veterinarian in most of the rest of the English-speaking world.

Ancient Indian sage and veterinarian Shalihotra (mythological estimate c. 2350 BCE), the son of a sage, Hayagosha, is considered the founder of veterinary sciences.[4]

The first veterinary college was founded in Lyon, France, in 1762 by Claude Bourgelat.[5] According to Lupton, after observing the devastation being caused by cattle plague to the French herds, Bourgelat devoted his time to seeking out a remedy. This resulted in his founding a veterinary college in Lyon in 1761, from which establishment he dispatched students to combat the disease; in a short time, the plague was stayed and the health of stock restored, through the assistance rendered to agriculture by veterinary science and art.[6]

The Odiham Agricultural Society was founded in 1783 in England to promote agriculture and industry,[7] and played an important role in the foundation of the veterinary profession in Britain.[8] A 1785 Society meeting resolved to "promote the study of Farriery upon rational scientific principles."
The professionalization of the veterinary trade was finally achieved in 1790, through the campaigning of Granville Penn, who persuaded the Frenchman Charles Vial de Sainbel to accept the professorship of the newly established Veterinary College in London.[7] The Royal College of Veterinary Surgeons was established by royal charter in 1844.

Veterinary science came of age in the late 19th century, with notable contributions from Sir John McFadyean, credited by many as having been the founder of modern Veterinary research.[9]
Veterinarians treat disease, disorder or injury in animals, which includes diagnosis, treatment and aftercare. The scope of practice, specialty and experience of the individual veterinarian will dictate exactly what interventions they perform, but most will perform surgery (of differing complexity).
Unlike in human medicine, veterinarians must rely primarily on clinical signs, as animals are unable to vocalize symptoms as a human would. In some cases, owners may be able to provide a medical history and the veterinarian can combine this information along with observations, and the results of pertinent diagnostic tests such as radiography, CT scans, MRI, blood tests, urinalysis and others.
Veterinarians must consider the appropriateness of euthanasia ("putting to sleep") if a condition is likely to leave the animal in pain or with a poor quality of life, or if treatment of a condition is likely to cause more harm to the patient than good, or if the patient is unlikely to survive any treatment regimen. Additionally, there are scenarios where euthanasia is considered due to the constraints of the client's finances.
As with human medicine, much veterinary work is concerned with prophylactic treatment, in order to prevent problems occurring in the future. Common interventions include vaccination against common animal illnesses, such as distemper or rabies, and dental prophylaxis to prevent or inhibit dental disease. This may also involve owner education so as to avoid future medical or behavioral issues.
Additionally, veterinarians can play important roles in public health and the prevention of zoonoses.[10]

The majority of veterinarians are employed in private practice treating animals (75% of vets in the United States, according to the American Veterinary Medical Association).[11]
Small animal veterinarians typically work in veterinary clinics, veterinary hospitals, or both. Large animal veterinarians often spend more time travelling to see their patients at the primary facilities which house them, such as zoos or farms.
Other employers include charities treating animals, colleges of veterinary medicine, research laboratories, animal food companies, and pharmaceutical companies. In many countries, the government may also be a major employer of veterinarians, such as the United States Department of Agriculture or the Animal and Plant Health Agency in the United Kingdom. State and local governments also employ veterinarians.[12][13]
The COVID-19 pandemic has created a greater demand for veterinary services.[14] Many people are home with extra time on their hands, and adoption agencies and animals shelters have seen a surge in pet purchases as a result.[14] The American Veterinary Medical Association has provided COVID-19 resources for veterinarians on prevention measures, animal testing, and wellbeing.[15]
Veterinarians and their practices may be specialized in certain areas of veterinary medicine. Areas of focus include:
Veterinary specialists are in the minority compared to general practice veterinarians, and tend to be based at points of referral, such as veterinary schools or larger animal hospitals. Unlike human medicine, veterinary specialties often combine both the surgical and medical aspects of a biological system.
Veterinary specialties are accredited in North America by the AVMA through the American Board of Veterinary Specialties, in Europe by the European Board of Veterinary Specialisation and in Australia and New Zealand by the Australasian Veterinary Boards Council.[19][20][21] While some veterinarians may have areas of interest outside of recognized specialties, they are not legally specialists.
Specialties can cover general topics such as anesthesiology, dentistry, and surgery, as well as organ system focus such as cardiology or dermatology. A full list can be seen at veterinary specialties.
Many veterinarians, especially in large animal practice, offer house calls and farm calls through a mobile practice. The start-up and operating costs of a mobile practice are typically lower than those of a traditional brick and mortar hospital, which can cost millions of dollars or more for equipment and surgical supplies. Costs associated with mobile units can range from as low as $5,000 for a utility box in an SUV to around $250,000 for a fully equipped custom built chassis.[22] The potential advantages to the client are not having to transport the animal, lower stress for the animal, a lower risk of disease transmission from other animals, and convenience. A 2015 study published in the Journal of American Veterinary Medical Association proved that blood pressure readings, pulse rates and body temperature rates were increased by 11–16% when those readings were done in the clinic versus in the home.[23] However, mobile practices often lack the facilities and equipment to provide advanced care, surgery, or hospitalization. Some mobile practices maintain a relationship with a traditional hospital for referral of cases needing more comprehensive care.
The last AVMA Report on Veterinary Compensation, published in 2018, indicated private practice associate veterinarians who had board certification earned a mean of $187,000. A veterinarian's salary can easily exceed $300,000 depending on the specialty. The median starting salary for new veterinary graduates without specialization in 2018 was $103,800 in the United States according to the Bureau of Labor Statistics, while the lowest paid earned less than $89,540 annually.[24] States and districts with the highest mean salary are California ($398,340), Michigan ($325,100), Illinois ($324,870), New York ($322,500), and Hawaii ($221,150).[25] Veterinarians who own their own clinics are typically paid a much higher salary. The average owner payout is $400,000 for every $1,000,000 of clinic income. In 2021 there were practices sold with $8–10,000,000 in yearly revenue with the owners drawing salaries of several million dollars. Over 90% of practice owners do not regret purchasing or starting their own practice, according to a 2020 survey of clinic owners.

In order to practice, vets must complete an appropriate degree in veterinary medicine, and in most cases must also be registered with the relevant governing body for their jurisdiction.
Degrees in veterinary medicine culminate in the award of a veterinary science degree, although the title varies by region. For instance, in North America, graduates will receive a Doctor of Veterinary Medicine (Doctor of Veterinary Medicine or Veterinariae Medicinae Doctoris; DVM or VMD), whereas in the United Kingdom, Australia, New Zealand or India they would be awarded a Bachelor of Veterinary Science, Surgery or Medicine (BVS, BVSc, BVetMed or BVMS), and in Ireland graduates receive a Medicinae Veterinariae Baccalaureus (MVB). In continental Europe, the degree of Doctor Medicinae Veterinariae (DMV, DrMedVet, Dr. med. vet., MVDr.) or Doctor Veterinariae Medicinae (DVM, DrVetMed, Dr. vet. med.) is granted.[26]
The award of a bachelor's degree was previously commonplace in the United States, but the degree name and academic standards were upgraded to match the 'doctor' title used by graduates.
Comparatively few universities have veterinary schools that offer degrees which are accredited to qualify the graduates as registered vets. For example, there are 30 in the United States, 5 in Canada, 1 in New Zealand, 7 in Australia (4 of which offer degrees accredited by the American Veterinary Medical Association (AVMA)), and 8 in the United Kingdom (4 of which offer degrees accredited by the American Veterinary Medical Association (AVMA)).[27]
Due to this scarcity of places for veterinary degrees, admission to veterinary school is competitive and requires extensive preparation. In the United States in 2007, approximately 5,750 applicants competed for the 2,650 seats in the 28 accredited veterinary schools, with an acceptance rate of 46%.[28]
With competitive admission, many schools may place heavy emphasis and consideration on a candidate's veterinary and animal experience. Formal experience is a particular advantage to the applicant, often consisting of work with veterinarians or scientists in clinics, agribusiness, research, or some area of health science. Less formal experience is also helpful for the applicant to have, and this includes working with animals on a farm or ranch or at a stable or animal shelter and basic overall animal exposure.[29]
In the United States, approximately 80% of admitted students are female. In the early history of veterinary medicine of the United States, most veterinarians were males. However, in the 1990s this ratio reached parity, and now it has been reversed.
Preveterinary courses should emphasize the sciences. Most veterinary schools typically require applicants to have taken one year equivalent classes in organic, inorganic chemistry, physics, general biology; and one semester of vertebrate embryology and biochemistry. Usually, the minimal mathematics requirement is college level calculus. Individual schools might require introduction to animal science, livestock judging, animal nutrition, cell biology, and genetics. However, due to the limited availability of these courses, many schools have removed these requirements to widen the pool of possible applicants.
Following academic education, most countries require a vet to be registered with the relevant governing body, and to maintain this license to practice.
According to the Bureau of Labor Statistics, veterinarians must be licensed to practice in the United States.[30] Licensing entails passing an accredited program, a national exam, and a state exam. For instance, in the United States, a prospective vet must receive a passing grade on a national board examination, the North America Veterinary Licensing Exam. This exam must be completed over the course of eight hours, and consists of 360 multiple-choice questions, covering all aspects of veterinary medicine, as well as visual material designed to test diagnostic skills.
The percentage electing to undertake further study following registration in the United States has increased from 36.8% to 39.9% in 2008. About 25% of those or about 9% of graduates were accepted into traditional academic internships. Approximately 9% of veterinarians eventually board certify in one of 40 distinct specialties from 22[31] specialty organizations recognized by the AVMA American Board of Veterinary Specialties (ABVS).[32][33]
Source:[34]
| Anesthesiology and analgesia | Animal welfare | Avian practice |
| Bacteriology and mycology | Beef cattle practice | Behavior |
| Canine and feline medicine | Cardiology | Dairy practice |
| Dentistry | Dermatology | Exotic animal medicine |
| Emergency and critical care | Equine medicine | Epidemiology |
| Laboratory animal medicine | Orthopaedics | Internal medicine |
| Pathology | Pharmacology | Poultry medicine |
| Reproductive medicine | Radiation oncology | Radiology |
| Shelter medicine | Surgery | Swine health management |
| Toxicology | Virology | Zoological medicine |
The first two-year curriculum in both veterinary and human medical schools are very similar in course names, but in certain subjects are relatively different in content. Considering the courses, the first two-year curriculum usually includes biochemistry, physiology, histology, anatomy, pharmacology, microbiology, epidemiology, pathology and hematology.[35]
Some veterinary schools use the same biochemistry, histology, and microbiology books as human medical students; however, the course content is greatly supplemented to include the varied animal diseases and species differences. In the past, many veterinarians were trained in pharmacology using the same text books used by physicians. As the specialty of veterinary pharmacology has developed, more schools are using pharmacology textbooks written specifically for veterinarians. Veterinary physiology, anatomy, and histology is complex, as physiology often varies among species. Microbiology and virology of animals share the same foundation as human microbiology, but with grossly different disease manifestation and presentations. Epidemiology is focused on herd health and prevention of herd borne diseases and foreign animal diseases. Pathology, like microbiology and histology, is very diverse and encompasses many species and organ systems. Most veterinary schools have courses in small animal and large animal nutrition, often taken as electives in the clinical years or as part of the core curriculum in the first two years.
The final two-year curriculum is similar to that of human medicine only in clinical emphasis.[35] A veterinary student must be well prepared to be a fully functional veterinarian on the day of graduation, competent in both surgery and medicine. The graduating veterinarian must be able to pass medical board examination and be prepared to enter clinical practice on the day of graduation, while most human medical doctors in the United States complete 3 to 5 years of post-doctoral residency before practicing medicine independently, usually in a very narrow and focused specialty. Many veterinarians do also complete a post-doctoral residency, but it is not nearly as common as it is in human medicine.
In the last years, curricula in both human and veterinary medicine have been adapted with the aim of incorporating competency-based teaching.[36][37] Furthermore, the importance of institutionalized systematic teacher feedback has been recognized and tools such as clinical encounter cards are being implemented in clinical veterinary education.[38]
Some veterinarians pursue post-graduate training and enter research careers and have contributed to advances in many human and veterinary medical fields, including pharmacology and epidemiology. Research veterinarians were the first to isolate oncoviruses, Salmonella species, Brucella species, and various other pathogenic agents. Veterinarians were in the forefront in the effort to suppress malaria and yellow fever in the United States. Veterinarians identified the botulism disease-causing agent, developed propofol; a widely used anesthetic induction drug,[39] produced an anticoagulant used to treat human heart disease,[40] and developed surgical techniques for humans, such as hip-joint replacement, limb and organ transplants.
Veterinarians work with a wide variety of animal species typically in hospitals, clinics, labs, farms, and zoos.[41] Veterinarians face many occupational hazards including zoonotic diseases, bites and scratches, hazardous drugs, needlestick injuries, ionizing radiation, and noise.[42][43][44] According to the U.S. Department of Labor, 12% of workers in the veterinary services profession reported a work-related injury or illness in 2016.[45]
Veterinary practices need a health and safety plan that addresses infection prevention and other hazards.[44][46] Workplaces should utilize engineering controls, administrative controls, and personal protective equipment to keep their employees safe.[46][44] PPE such as gloves, safety goggles, lab coats, and hearing protection should be readily available with mandatory training on proper usage. Raising awareness is the most important step in promoting workplace health and safety.[45]
Needlestick injuries are the most common accidents among veterinarians, but they are likely underreported.[45][46][47] Needlesticks can result in hazardous drug or bloodborne-pathogen exposures.
Unlike human medical professionals, veterinarians receive minimal training on safe handling of hazardous drugs in school.[48] Also, a large percentage of veterinarians are women of reproductive age and drug exposures put them at risk of infertility or other adverse health outcomes.[48][49] Additionally, some antibiotics, steroids, and chemotherapy drugs are known to have negative effects on male fertility.[50] The U.S. National Institute for Occupational Safety and Health has issued guidance on the safe handling of hazardous drugs for veterinary workers.[51] Animal bites and scratches are another common injury in veterinary practice.[43]
The close interactions with animals put veterinarians at increased risk of contracting zoonoses. A systematic review of veterinary students found that between 17% and 64% had acquired a zoonotic disease during their studies.[42] The animal species, work setting, health and safety practices, and training can all affect the risk of injury and illness.[42]
Noise can be a prominent exposure, in which case a hearing loss prevention program may be recommended. A NIOSH study on kennel noise found that noise levels often exceeded OSHA's permissible exposure limit.[52] Reducing noise is beneficial for animal and human health.[53][54]
Veterinarians have high suicide rates in comparison to the general population.[55] A study by the U.S. Centers for Disease Control and Prevention found that male veterinarians are 2.1 times and female veterinarians are 3.5 times as likely as the general population to die by suicide.[55] Some reasons for this could be long hours, work overload, client expectations and complaints, poor remuneration, euthanasia procedures, and poor work-life balance.[55] A survey of more than 11,000 vets found 9% had serious psychological distress, 31% experienced depressive episodes, and 17% had suicidal ideation.[56] Online support groups, such as Not One More Vet, have been established to help veterinarians who may be experiencing suicidal thoughts.[57] NOMV educates veterinarians and vet techs about other ways to help themselves with mental health.[58] Another driver of stress can be student loan debt. A 2013 national survey found that average debt for veterinary medicine graduates was as high as $162,113.[59] Veterinarian lifelong earning potential is less than a physician, so it can take a lot longer to break even.[59]
Reality televisions shows featuring veterinarians include:
Fictional works featuring a veterinarian as the main protagonist include:
Most states in the US allow for malpractice lawsuit in case of death or injury to an animal from professional negligence. Usually the penalty is not greater than the value of the animal. Some states allow for punitive penalty, loss of companionship, and suffering, likely increasing the cost of veterinary malpractice insurance and the cost of veterinary care. Most veterinarians carry business, worker's compensation, and facility insurance to protect their clients and workers from injury inflicted by animals.[citation needed]
I am leaving this review almost a year after my Golden Doodle, Kahlua had passed from Lymphoma. When she was diagnosed with Lymphoma by our local vet, and told she had maximum a month to live, we decided to consult with an Oncologist at BBVSH. We were fortunate to get Dr Kirsten Elliot. From my initial consultation with Dr Elliot to the duration of her treatments, which consisted of two (5 round treatments), I felt Dr Elliot was genuinely passionate about giving her terminal patients the best care there is. Knowing how devastated I was and wanting to find a treatment to prolong Kahlua's life without sacrificing quality of life, she presented me with many options and honest on what the probability of success with each option. Chemo Treatment is very expensive and she said it was okay if we just wanted to do palliative care instead. She offered information and professional advice, but never pressured me into anything. I chose a treatment plan that was doable cost-wise that could have a high probability of success without sacrificing her quality of life. I am grateful for her help in giving Kahlua almost 2 extra years with us. Kahlua went into remission during treatment, but came out of it a year and a half later, then a 2nd round, which put her back in remission. Kahlua went through the chemo treatments well, and lived out her last 2 years normally, being the outdoor hiking, biking trail girl in the forest. .. til the cancer took over again. Thank you to Dr Elliot and the team at BBVSP. They were wonderful in taking care of Kahlua. Dr Elliot was caring, kind, professional, compassionate, and made the whole process as comfortable as can be for Kahlua. I highly recommend Dr Elliot and the BBVSH team if ever in need of Oncology care.
Our dog has had 6 surgeries with these guys. The surgeons are beyond excellent. They take the time to fully explain and are always there if you need them. You know when you are freaking out over swelling and call in a panic. They will always answer your call with patience and their wisdom. Highly recommend them. They are expensive!
I had an extremely frustrating experience at Boundary Bay Animal Emergency that felt more like a money scam than genuine veterinary care. I took my young cat there after he hadn’t eaten for three days and was acting strangely. I suspected he had an obstruction, but after paying the $275 consultation fee, the vet didn’t even check his throat. Instead, they proposed sedation and an X-ray for an outrageous $1,400, which was significantly higher than other emergency clinics I’ve visited. Unable to afford that, I went home and, with a flashlight, found the obstruction myself. I managed to remove it, which left me questioning why the vet and assistant didn't check his throat first. This situation could have been dire for my cat, and I feel the clinic prioritized profit over care. I cannot recommend this place unless you’re prepared to spend a lot without thorough examination. Definitely go elsewhere if you value your pet's life over filling their pockets. Photo of obstruction with a loonie to show size.
I cannot say enough wonderful things about Dr. Judy Rochette and the staff at Boundary Bay. The service we experienced was top notch! Yes, you pay for it. But when your pet is in crisis you want to know that they are in the best hands. Specialists aren't always known for having the best bedside manner but Dr. Rochette is very down to earth, friendly and compassionate, and was very respectful and honouring of my wishes when it came to devising my pup, Winston's, care plan. Communication was a priority and regular updates were given during Winston's stay. I was invited to call anytime with any questions and visits were encouraged. I would highly recommend Boundary Bay for beloved pets needing specialized care.
We're looking into whether there are language support services for non-English speaking pet owners during an emergency visit. It's crucial for everyone to understand their pet's needs and the care they're receiving.
We prioritize every pet's health, so for non-life-threatening emergencies like dental issues, we assess and provide immediate care to alleviate pain and prevent further complications, ensuring they're stable before recommending further treatment or specialist care.
We're curious if they provide complementary therapies or holistic treatments in their emergency care. It'd be reassuring to have access to such options, ensuring our pets receive the most well-rounded care possible during emergencies.